Antibiotic resistance is a scary concept, but at least there’s comfort in seeing so many great minds trying to solve the problem. Last week’s announcement that President Obama had issued an executive order for the development of a national plan to battle antibiotic resistance dovetailed nicely with a paper just published in Science Translational Medicine from NIH scientists.
The publication, “Single-molecule sequencing to track plasmid diversity of hospital-associated carbapenemase-producing Enterobacteriaceae,” reports the sequencing of 20 isolates of Enterobacteriaceae resistant to carbapenems, a powerful class of antibiotics used as a last resort in hospitals. Lead author Sean Conlan from NHGRI and his collaborators used the sequence data to understand the transmission path of a Klebsiella pneumoniae outbreak at the NIH Clinical Center in 2011, as well as isolates collected after the outbreak ended.
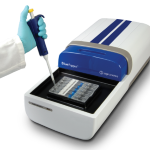
It’s impressive work, and we’re happy to report that our BluePippin automated DNA size selection platform was used in the project. Sequencing was performed with the PacBio RS II DNA Sequencing System; the team used BluePippin to remove fragments smaller than 5 Kb from the library prior to loading on the sequencer.
Long reads were necessary for the project, the authors note, because short-read sequence data as well as strain-typing technologies were unable to clearly distinguish between the organisms or to fully assemble the genomes.
Conlan et al. report finding less horizontal gene transfer than expected, but having the full sequence — including the drug-resistance-encoding plasmids associated with each genome — enabled them to get a sense of the remarkable diversity of the network of plasmids available to these bacteria.
The team also discovered that most of the cases suspected to represent hospital-acquired infections were in fact acquired earlier and missed in routine screening. This information helped them to focus their infection-prevention efforts on better screening at admission and increasing the frequency of surveillance cultures.
The authors suggest that real-time, whole-genome sequencing is already cost-effective for monitoring drug-resistant bacteria in clinical environments. “The cost of whole-genome sequencing is dwarfed by … costs associated with outbreaks and their investigations, including the human and financial toll and the loss of patient confidence in the health care facility,” they write.